Is that wisdom? That deep, penetrating gaze that looks around at its parents and the world as if it has seen it all before?
Today’s writing expedition comes on the heels of attending several births over the span of a week. There’s a buzz that accompanies this particular primal experience, surrounded as it is in liminal mist. I’m still tingling in the dew.
It also comes after a long walk along the shores of West Seattle during which I was, yet again, spiritually and intellectually tickled by an episode of the On Being podcast.
In this cast, host Krista Tippett has a conversation with multi-artist Joy Harjo, Muscogee Creek Nation member and 23rd Poet Laureate of the United States.
Have you ever sat reading a book when suddenly a single line or a statement jumps out at you with an eerie deja vu? The writer has captured your thoughts exactly. The conversation with Harjo was like that. In that way of deep see-ers and visionaries, the artist articulates something I have felt for as many years as I’ve watched babies being born:
We are all emerge from the womb knowing.
I have come to believe that we humans (and I have to assume all sentients) come into this world with all the wisdom and moral direction needed for a full and happy life. When I look into the sage eyes of a newborn, I feel sure a complete “how to” book on the universe is staring back at me, a step-by-step guide for how to benefit and live and love each other and the planet.
Harjo has witnessed the same thing. In her book Crazy Brave: A Memoir, she is more succinct on the matter: “We have instructions and a map buried in our hearts when we enter this world.”
Eventually, an infant’s innate knowing slips under the synaptic current that guides human development. It falls pray to restrictions and external influence and education and, for some, religion. That original book of knowing gets buried in a library of new sensations, information, doctrine, and politics. But as Harjo — and, it turns out, Yale researchers — points out, it takes a while for babies to lose site of what they innately know.
A lifelong storyteller suggests, Harjo says she has noticed it takes time to un-remember the ongoing stories newborns bring into this world from the place the inhabit before birth.
“I’ve always tried to get there when a grandchild is being born,” Harjo tells Tippett. “And what I’ve noticed — and I’ve noticed this with newborn infants — is they still remember. They’re still carrying memories and stories. They still know things. Even when they’re young — I remember my daughter skipping up to me when she was three. She used to say, ‘When I used to be a boy . . .’”
I am one of those people who stands always at the edge of scientific verification and spiritual possibility. So, while I haven’t found any empirical evidence that we “exist” somewhere else before conception and birth, and my logical side says we don’t, my dominant spiritual side is drawn to the possibility. Hope on it in fact.
Equally, I am drawn to the hope of our continued existence in some form after death. Which is why I was comforted by an article in National Geographic I read a couple years ago. It said, in essence, that the air embodied by our ancestors remains with us. In other words, we are breathing their presence, the very air they breathed.
The logic center of my mind has certainly wrestled with the spiritual and metaphysical centers — I mean, even I thought I was a little woo-woo for constantly seeing and feeling the presence of the newborn’s “deep knowing.” Little did I know it’s a full on theory with an official name: Innatism.
Thankfully hypothesizing has its measure in scientific rigor. Which is why, after listening to the Tippet-Harjo dialogue, I let me fingers do some walking along the information highway. Driving back a few years I ran across an article in Scientific American that highlights fascinating research into this question of what newborns know:
In the article, Yale researcher Paul Bloom outlines specific moral principles present at birth and exhibited in very early childhood. The list includes:
“An understanding that helping is morally good, and that harming, hindering, or otherwise thwarting the goals of another person is morally bad.”
“A rudimentary sense of justice—an understanding that good guys should be rewarded and bad guys should be punished.”
“An initial sense of fairness—in particular, that there should be an equal division of resources.”
“And alongside these principles are moral emotions, including empathy, compassion, guilt, shame, and righteous anger.”
Since then, work in other labs has shown infants arrive with a suitcase of values and intelligence, including intuitive physics.
"We believe that infants are born with the ability to form expectations and they use these expectations basically to predict the future," said Kristy van Marle, an assistant professor in the Department of Psychological Sciences at the University of Missouri in a report on her research.
Well, Whew! I am certainly woo-woo in a lot of areas. I love my tarot deck and iconography. But I’m glad to know I am not alone in my reversal “tabula rasa” thinking, the dominant theory on knowledge that I grew up with. The tabula rasa theory says we are but “blank slates” when we are born, sans any mental content whatsoever. Knowledge or intelligence, according to tabula rasa thinking, is only acquired from experience or perception.
(Speaking of knowledge, did you know woo-woo is actually in the dictionary? Oxford defines it as “unconventional beliefs regarded as having little or no scientific basis, especially those relating to spirituality, mysticism, or alternative medicine.” So much of what I pursue fits into that definition.)
This rabbit hole question of whether or not we are born knowing the secrets of a happy and healthy life or are simply empty vessels whose morality is painted in by on-planet experience and exposure is miles deep and millenniums long. It winds through most major philosophers, all world religions and every person who has ever gazed into the eyes of a newborn.
Is that wisdom? That deep, penetrating gaze that looks around at its parents and the world as if it has seen it all before?
It’s also a wide rabbit hole, what with all the other questions that the question of innate knowing begs. For example are the sense of knowing and knowledge the same thing? Is intuition knowledge? At what point are experience and perception defined as experience and perception? What does it mean to exist?
Still the science that says we do arrive with a moral sense of goodness, justice and fairness and with innate compassion and empathy has me asking a different set of questions.
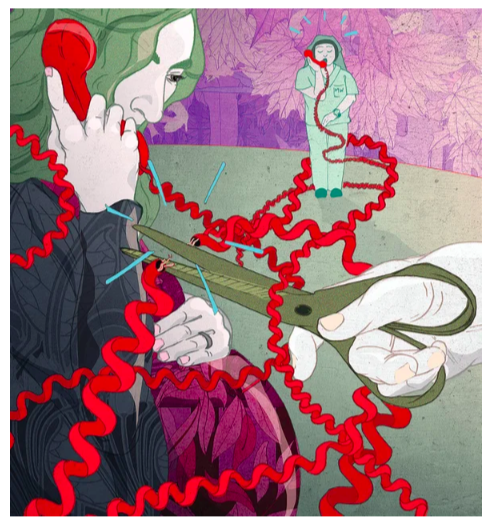
When and how does what we know coming into the world turn into racism, cruelty, greed, inequity, power-mongering, and all the things that are destroying humanity and the planet? How can we help our babies hang onto their innate moral maps as the navigate through a life and world of conflicting feelings, input, spiritual beliefs, and information?
I look at a newborn baby and I see the potential for world peace. How do we harness that potential?
Tippet’s conversation with Harjo does not go that far down the rabbit hole. But the artist’s phrasing regarding what we know before birth, as well as what we know after death, rings true to me. I have no empirical evidence, so of course my logical side whines in the background. But what the artist says rings true to what I have felt in the labor room:
“It’s wisdom beyond what our mentality, our Earth mental minds, our Earth mentality. It’s much larger and more immense than Earth mentality.”
I have to believe that we are born with stays with us. It’s in there, even in the cruelest of people. Perhaps what I see on the face of babies just entering the world is simply an infinite potential to save the world. If they can hang on to what they already know.
I love the image that Harjo presents of herself before she was born. And, I have to admit, I love the woo-woo idea that, likewise, each of us is enticed by something here on Earth, something that makes us willing to make the journey from wherever “there” is into our mother’s womb and out into the world.
“Though I was reluctant to be born, I was attracted by the music. I had plans… I did not want to leave mystery, yet I was ever curious and ready to take my place in the story.”
I am pretty sure the siren’s song for me was the desire to look in the eyes of babies.